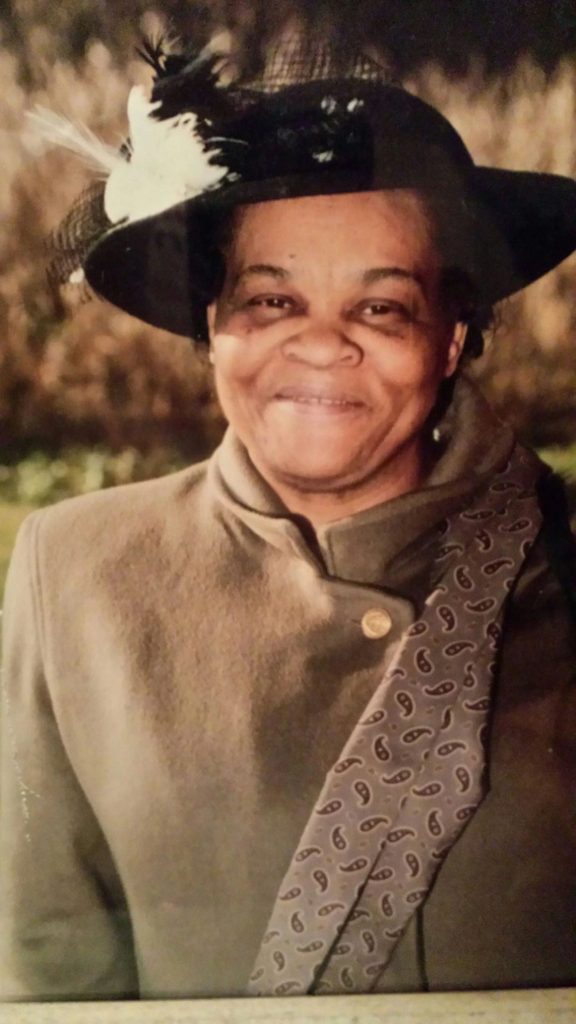
Receiving the Changemaker Award from the NYPENN Girl Scouts on behalf of Excellus BlueCross BlueShield was a deeply personal moment for Robyn Smith, CNY senior community investment and partnerships manager. It not only recognized the health plan’s commitment to health equity but also resonated with her own life experiences. In this feature, we connected with Robyn to explore her journey, the importance of the award, and her passion for supporting the LGBTQ+ community.
Q: Can you tell us about your family and the role they play in your life?
Robyn: Growing up, my immediate family was everything to me. I’m the youngest of four, with two sisters and a brother. My parents valued family, even though we didn’t have many extended family connections. We shared dinners regularly and spent weekends together, which created strong bonds. Those moments in the kitchen, filled with conversations and laughter, shaped my childhood. When I became a mother at a young age, it changed my perspective on life. My child inspired me to see the world differently and made me realize the importance of responsibility and love.

“Robyn’s story exemplifies the importance of love, family, and the need for safe spaces so that all young people can thrive! I am so proud that our organization and communities are made up of passionate, dedicated individuals like Robyn, who live our values every day. This Changemaker Award highlights our continued commitment to ensuring everyone feels welcomed, valued, respected and has fair opportunity to fully participate and reach their fullest potential. Engaging our communities, creating connections, and showing up for one another helps us meet our mission and drive better outcomes for all,” said Sady Alvarado-Fischer, Vice President, Diversity, Equity and Inclusion Officer at Excellus BlueCross BlueShield.
Q: What motivated you to get involved in LGBTQ+ pride events?
Robyn: I have two children who are part of the LGBTQ+ community. Through them, I’ve seen the challenges faced by this community, and I want to help. It’s important for me to contribute to ensure that everyone feels seen, heard, and loved, especially those who face discrimination.
Q: How did it feel to receive the Changemaker Award from the NYPENN Girl Scouts’ Beyond Programs for LGBTQ+ Youth, which was supported by a Health and Wellness Award from Excellus BCBS?
Robyn: Honestly, I became emotional. This recognition means a lot to me because of my family’s experiences and the challenges my children have faced. It reminds me how fortunate I am to work with organizations that do important community work. I hope our efforts help other families feel a sense of belonging.

Q: Why is it crucial to create safe spaces for LGBTQ+ youth?
Robyn: One of my children went through some tough times, including feelings of isolation and self-harm. It was heartbreaking to see them struggle. When we found ACR Health’s Q Center, it was like a light turned on for them. They found a safe place where they could be themselves, make friends, and experience moments that honored who they are. Safe spaces are essential for youth to feel supported and accepted.
Q: How does supporting LGBTQ+ initiatives relate to overall wellbeing?
Robyn: Mental health is a crucial part of well-being. By investing in LGBTQ+ programs, we provide resources that individuals may not have otherwise. It’s also important to find healthcare providers who understand the unique needs of the LGBTQ+ community, especially for minors. Knowing that our health plan supports these needs is invaluable.
Q: How do employee resource groups (ERGs) contribute to an inclusive workplace?
Robyn: Our employee resource groups (ERGs) and community investments are vital for creating a more inclusive environment. They give employees a platform to connect, share experiences, and support each other. By supporting initiatives that align with our values, we extend our commitment to diversity into the community, which strengthens our ties and demonstrates our social responsibility.
Q: What are your hopes for the future of LGBTQ+ advocacy?
Robyn: Today, navigating issues around gender identity and sexuality can be difficult. My hope is simple: people are people, love is love, and family is family. Everyone deserves to be respected for who they are, and we should embrace our shared humanity, without judgment.