“A close friend once told me that I was a people person and should use that ability as a social worker,” Megan Bunce recalls.
That advice, shared more than 15 years ago, led Megan to a career that has improved hundreds of children’s lives. Megan, a licensed social worker at Excellus BlueCross BlueShield, works with some of the most vulnerable people in our society.
She began her role in the Foster Care Program in 2023. Each year, this team provides case management to more than 1,000 children. More than that, though, the program provides stability, hope and a chance for a healthier future in a system that includes over 25,000 boys and girls in New York State.
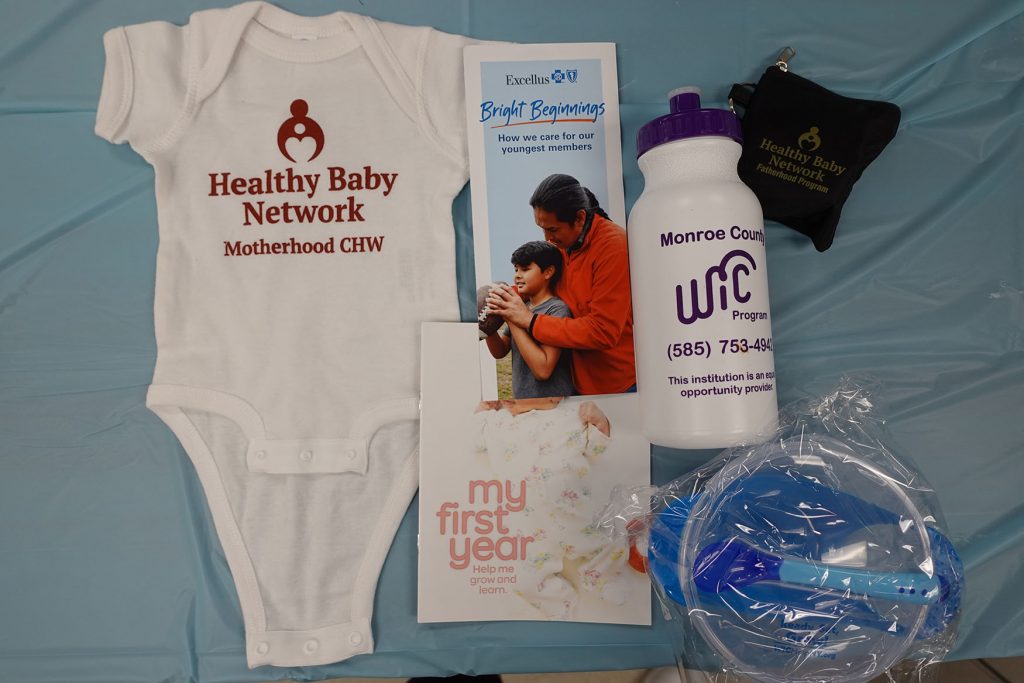
Supporting Our Youngest Members
Excellus BCBS may be best known for offering health plan options, but the nonprofit prides itself in its wide-ranging work around access and quality care. That includes children in foster care.
“I remember helping a little girl who had been struggling with her vision for years,” Megan recalls. “Together with her foster care case manager, we identified a provider, got the coverage approved and lined up the appointment where she was prescribed glasses. This may seem simple to some, but it’s often these types of things people take for granted that make a significant difference in a child’s life.”
The Foster Care team ensures medications are being used properly, vaccines are completed, and well-child visits are scheduled. Staff members also address any other gaps in care that may arise.
While the work is rewarding, it can often be difficult, according to Lindsay Rachow, a licensed mental health counselor and manager of the Foster Care Program. “As you can imagine, these young members’ stories can be challenging to read,” she says. “It takes a special person to serve in this role. Megan’s ability to connect with people is what makes her work so impactful.”
Megan appreciates that her work is seen and felt. “Never have I looked back and regretted the decision to move forward with this career,” she says.
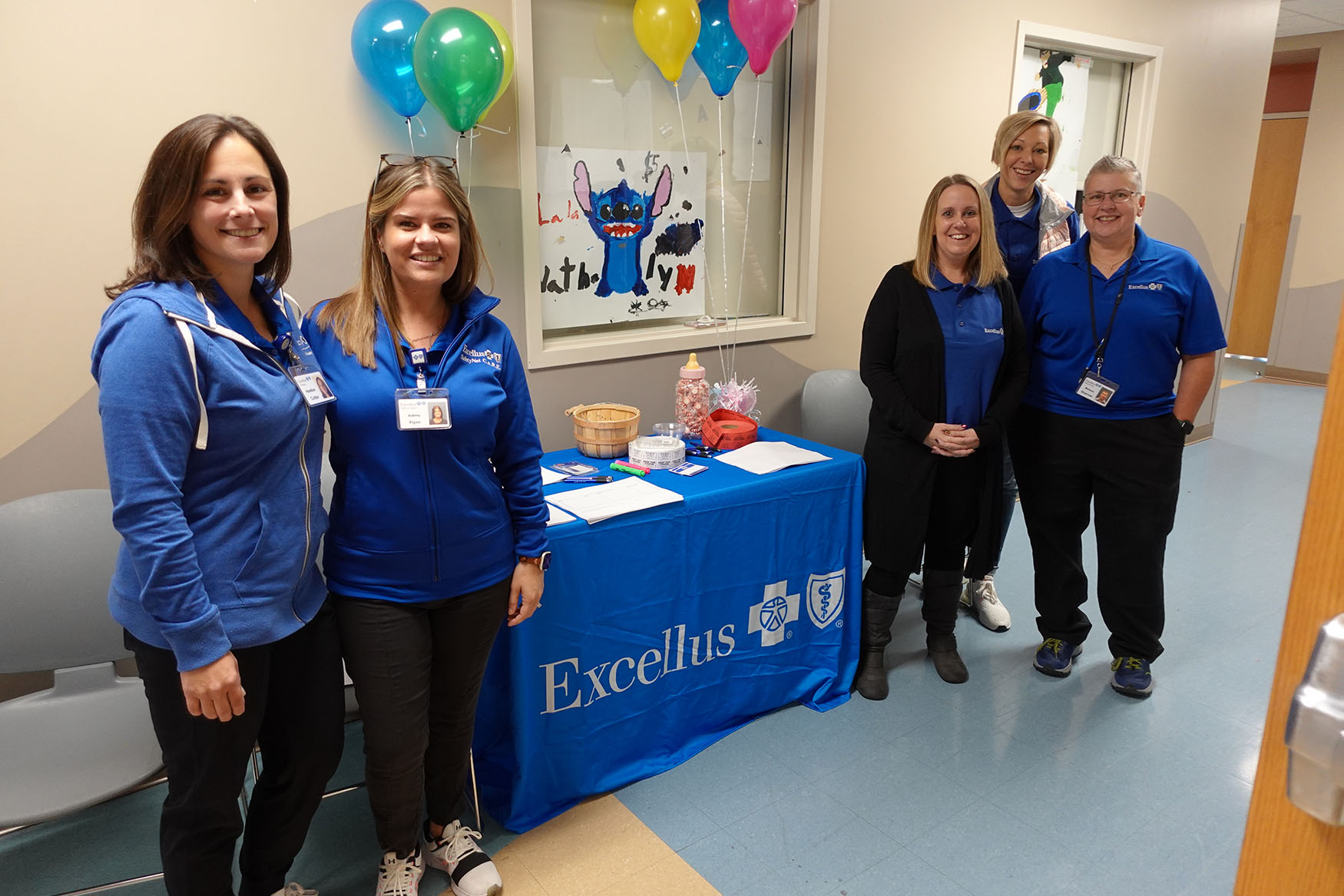
Building Effective Partnerships
JeanMarie Armellino, a social worker from the Children’s Home of Wyoming Conference, understands the complexity of these children’s needs. “Our continuous communication with the foster care team empowers us to respond swiftly to the children’s needs while fostering a more integrated approach to care,” she says.
The partnership with local foster care programs began in 2013, when Excellus BCBS launched an initiative to ensure children in foster care receive necessary services and support.
“Too often, the challenges faced by those aging out of the foster care system can lead to housing instability, unemployment and substance use,” Lindsay says. “The need for comprehensive support throughout their life is critical.”
For example, when the Excellus BCBS Foster Care Team receives a notification that a member in its care has had an emergency department or inpatient hospital visit, staff members take immediate action. They seek to understand the reason for the visit, providing education on urgent care versus emergency visits and ensuring that safety planning, medication changes and follow-up care are in place.
“Teamwork allows us to become a trusted resource for families, filling gaps in care and providing support during critical transitions,” Megan explains.
Impacting Health Outcomes Across New York State
Children in foster care are twice as likely as other children to have learning disabilities, three times more likely to have ADD or ADHD and seven times more likely to suffer from depression. These alarming statistics underline the necessity of the services that Excellus BCBS provides.
“Youth in the foster care system often face unique social determinants of health challenges,” Megan says. “It’s common for them to have higher rates of mental health conditions like anxiety and depression, as well as chronic health issues like obesity to asthma. They’re at a greater risk for a myriad of health problems compared to their peers. Our work is vital.”
Both Megan and Lindsay say their support extends beyond case management. They offer training to foster parents, encouraging them to attend the Children’s Advisory Committee meetings held twice a year, covering topics like substance use and self-care for caregivers. They also ensure that children’s wishes are considered when making decisions about their medical needs, working closely with caseworkers to respect each child’s voice.
“The work we are doing serves as a powerful reminder that when we come together to support one another, we can create lasting change and brighter futures for those who need it most,” Megan says. “I have found meaning in being the person families could rely on. When they look back, they can say, ‘Megan was there for our family’ — those are the moments I will never forget.”
To learn more about the Foster Care Program at Excellus BCBS, visit excellusbcbs.com.